Kunte H, Kunte G, Busch MA, Weichert W, Rueckert RI, Harms L (2010): Differences in carotid plaque content of macrophages, T cells and MMP-9 between patients with embolic and hemodynamic cerebral ischemia due to symptomatic carotid stenosis
Atherosclerosis 211 (2): 456-460. Epub Mar 9. doi: 10.1016/j.atherosclerosis.2010.03.005.
Background
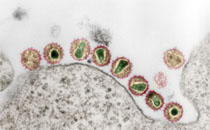
Cerebral ischemia in patients with carotid artery atherosclerosis is most often caused by thromboembolism, while hemodynamic stroke mechanism is rare. Differences in plaque inflammation according to stroke mechanism are an understudied issue. The purpose of this pilot study was to compare carotid plaque inflammation in patients with thromboembolic and hemodynamic cerebral ischemia.
Methods
We included 6 patients with hemodynamic and 27 with embolic cerebral ischemia who had carotid endarterectomy (CEA). We compared plaque morphology markers (macrophages, T cells, MMP-9, plaque rupture, surface thrombus, intraplaque hemorrhage, lipid core) between patients with hemodynamic and embolic cerebral ischemia and assessed vascular events and deaths during the first year post CEA.
Results
Compared to patients with hemodynamic mechanism, those with embolic mechanism showed a higher median (interquartile range) content of T cells/mm2 [49.66 (21.26–71.39) vs. 10.28 (7.05–13.87); P = 0.0005] and higher median total percentages of macrophage area [2.81% (1.69–4.09) vs. 0.99% (0.57–1.50); P = 0.003] and MMP-9 area [0.63% (0.42–1.01) vs. 0.25% (0.05–0.45); P = 0.007]. Signs of plaque instability such as plaque rupture, surface thrombus and intraplaque hemorrhage showed a tendency to be more pronounced in patients with thromboembolism. The incidences of vascular events and the survival rates in the first year after CEA were similar in the two groups.
Conclusions
Major differences in plaques related to stroke mechanism were found in patients with symptomatic carotid stenosis. However, further investigations are necessary to validate our results. Identification of stroke mechanism may improve risk stratification and could help to identify the most suitable secondary stroke prevention strategy.